Team II Genome Assembly Group: Difference between revisions
| Line 27: | Line 27: | ||
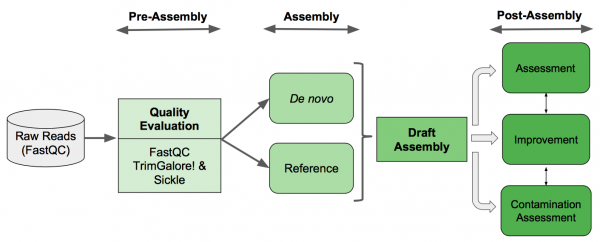
== Genome Assembly Pipeline == | == Genome Assembly Pipeline == | ||
[[File: 4.png ]] | [[File: 4.png | 600px]] | ||
== Pre-Assembly == | == Pre-Assembly == | ||
Revision as of 00:36, 5 March 2018
Introduction
Background
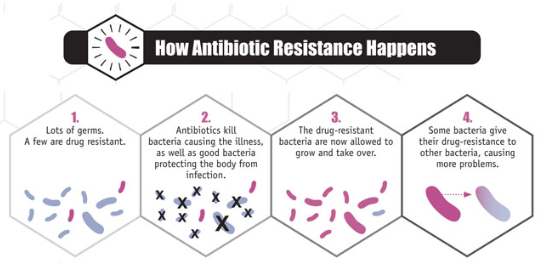
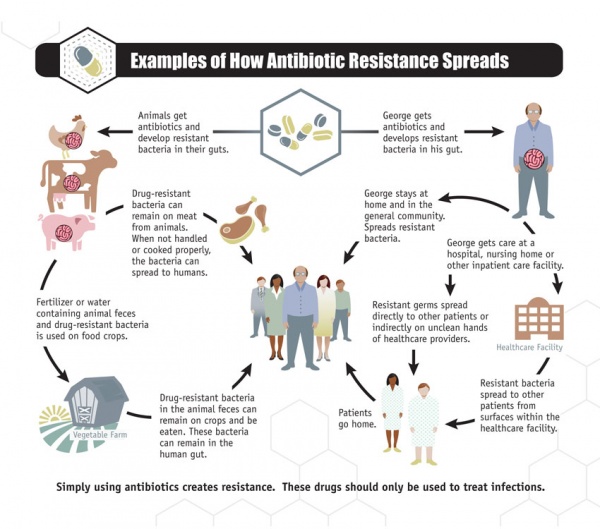
Antibiotic resistance has been called one of the world’s most pressing public health problems. Antibiotic resistance is the ability of bacteria to resist the effects of an antibiotic. It occurs when bacteria change in a way that reduces the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. The bacteria survive and continue to multiply, causing more harm (Figure 1.a.). Antibiotic resistance can cause illnesses that were once easily treatable with antibiotics to become dangerous infections, prolonging suffering for children and adults. Antibiotic-resistant bacteria can spread to family members, schoolmates, and co-workers, and may threaten your community (Figure 1.b). Antibiotic-resistant bacteria are often more difficult to kill and more expensive to treat and in some cases, can lead to serious disability or even death [1].
Figure 1: a. How antibiotic resistance happens, b. How antibiotic resistance spreads
Data
Emory Antibiotic Resistance Center (ARC) in Emory University, School of medicine tries to better understand antibiotic resistance to combat this crisis and improve human health. Their goals include learning how antibiotic resistance develops, optimizing the way antibiotics are used to preserve their power, and discovering novel therapeutics and vaccines to directly combat antibiotic-resistant pathogens. Solving the crisis of antibiotic resistance requires a multi-faceted approach that crosses traditional boundaries [2].
They Provided us with a sample of 262 pair-end raw reads sequencing of Klebsiella spp, from illumina MiSeq.
Klebsiella is a genus of nonmotile, Gram-negative, oxidase-negative, rod-shaped bacteria (Figure 2) with a prominent polysaccharide-based capsule. Klebsiella species are found everywhere in nature. The members of the genus Klebsiella are a part of the human and animal's normal flora in the nose, mouth and intestines. The species of Klebsiella are all gram-negative and non-motile. They tend to be shorter and thicker when compared to others in the Enterobacteriaceae family. The cells are rods in shape and generally measures 0.3 to 1.5 µm wide by 0.5 to 5.0 µm long. They can be found singly, in pairs, in chains or linked end to end. Klebsiella can grow on ordinary lab medium and do not have special growth requirements, like the other members of Enterobacteriaceae. Some of Klebsiella types are: K.granulomatis, K. oxytoca, K. michiganensis and K. pneumoniae (type-species: K. p. subsp. ozaenae, K. p. subsp. pneumoniae, K. p. subsp. rhinoscleromatis) [3]. Though, they have been extensively studied, for example, only four complete genomes of K. pneumoniae were available till 2011 [4]. To better understand the multidrug resistance factors in Klibsiella, we need to determine genome DNA sequences of strains.
Figure 2: Scanning electron microscope image of Klebsiella pneumoniae. From: Bioquell.com
Objectives
- To distinguish between susceptible and heteroresistant strains/species
- To discover genomic determinants of antibiotic resistance
- To develop a predictive web server